Having SRT treatment
Stereotactic radiotherapy to the brain
Starting your treatment
When you arrive for your appointment, please book in at reception in the Radiotherapy Village on Level R.
We will show you to a cubicle where you can change into a gown.
When you are ready, we will take you into the treatment room. You will need to lie on the scanning table. It will be set up with the same equipment as when you had your CT scan.
We will fit your mask over your face and secure it in place.
The lights will be dimmed. This is so the radiographers can see the room lasers to make sure you are in the correct position. Try to stay still, relax and breathe normally.
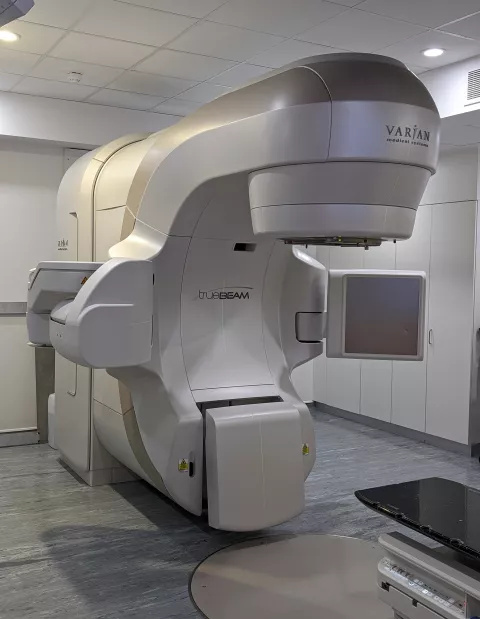
The radiotherapy machine is called a linear accelerator, often referred to as a linac. You will hear the machine move around you. It will come close to you but will not touch you. You will hear radiographers taking various measurements and feel the bed moving.
To make sure you are in the right position before your treatment, we use a piece of equipment called AlignRT. It also makes sure you are in the right position every time you have radiotherapy treatment. Once you are in the right position, the radiographers will leave the room.
You will hear a buzzing sound which is the door safety interlock. You will be alone in the room during your treatment but the radiographers will be watching you all the time on CCTV.
We will take X-ray images during your treatment to make sure that the treatment is being delivered accurately. There will be a short delay while these images are checked. You might feel the bed move as the radiographers adjust its position from outside of the room.
Once treatment starts, the machine will move around you to treat you from different angles. It will take about 1 hour.
When treatment has finished, the radiographers will come back in to the room. They will remove your mask.
The treatment table will be quite high up so you should wait until the radiographers tell you it is safe to get off the table.
After your treatment
The radiographer will talk to you about what to expect and how to look after yourself after your treatment. They will make sure you have the correct medicine to take home with you.
You can then go home. You shouldn’t fell unwell, but we do recommend that you have a responsible adult to travel home with you.
Driving
There are some medical conditions that can affect your driving. If your doctor has told you that you should not drive you must tell the DVLA.
You can find more information on the GOV.UK website.
The Brain Tumour Charity also has useful information and support for those who need to surrender their driving licences.
Washing
It is important to keep the treatment area clean. Shower or bathe using lukewarm water and use your usual shampoo. Use a soft towel to gently pat the skin dry. Do not rub.
Swimming
Reduce the number of times you swim in chlorinated water as this can have a drying effect on the skin. After swimming, shower to remove excess chlorine. Stop swimming if the skin becomes sore.
Side effects of SRT treatment
Read more about the possible side effects from having SRT treatment.
Tiredness
You might feel tired for a few weeks after your treatment. This is usually temporary.
Swelling
There is a risk of swelling developing around the area that is being treated. To reduce this risk, we might prescribe a course of steroids (dexamethasone) for you. If you are already taking this steroid medicine, we might advise that the dose needs to be temporarily increased.
We will explain how to take your steroid medicine. You might also be given medicine to protect your stomach from irritation caused by the steroid.
Skin reaction
Treatment to tumours close to the surface of the skin can cause a reaction over the area being treated. The area might become red, dry, sensitive or begin to peel.
Moisturising the treatment area will help. You can continue to use your usual moisturiser. If you need to buy one, we recommend one without the additive, sodium lauryl sulphate (SLS). After treatment, apply the moisturiser sparingly 2 times a day or more often if your skin is very itchy.
Hair loss
Losing hair happens with nearly all radiotherapy treatments to the head. It varies from person to person on how much hair you lose. It will only happen in small patches where the treatment has been directed. Hair loss is less likely with SRT.
We will explain if this is likely to happen and where to expect some hair loss. Hair usually starts to grow again around 4 to 5 months after treatment. It is unlikely that you will have significant permanent hair loss.
If you feel conscious about your hair loss, we can arrange for you to be fitted with a wig on prescription.
Seizures or fits
There is a slight increased risk that you might have a seizure (fit) after your treatment. This is more likely if you have had seizures in the past. Your neuro-oncology team will discuss the chances of you having a seizure and what to do if this happens.
Feeling sick (nausea)
You might feel sick and feel dizzy after your treatment. This can last for about 2 weeks. We will give you advice on how to cope with this. We might prescribe some anti-sickness medicine for you.
Possible long-term side effects
Long-term side effects can happen many months or years after radiotherapy has finished. These later side effects are hard to predict. If you do get them, they can sometimes be permanent.
We carefully plan our treatment to avoid the surrounding areas of the tumour as much as possible. This reduces the chance of these side effects, which are generally very rare. If the tumour is close to the pituitary gland, hormonal changes might occur. This will be closely monitored. As the treatment kills the tumour (causes necrosis), this might need surgery or additional medicine in a few patients.
All treatments will leave some scarring in the brain (gliosis). Some areas of the brain are more sensitive than others. This will be monitored by your clinical team.
A further brain tumour
There is a very rare chance of developing another tumour as a result of radiotherapy treatment. This happens in less than 1 in 1,000 people treated and usually develops 10 to 20 years after radiotherapy treatment has been completed.
Vestibular schwannoma treatment only
If you are having treatment for a vestibular schwannoma, you might develop some numbness in your face. This does not usually last long and occurs in 1 in 30 people (3%).
Some weakness in your face might happen. This usually improves but, in less than 1 in 50 people (2%) treated, long-term weakness in the face can happen.
If your vestibular schwannoma is very large, there is a risk of swelling affecting the flow of fluid through your brain. One in 20 people (5%) might need to have a shunt inserted by a neurosurgeon. The shunt helps to drain away cerebro-spinal fluid (CSF).
One in 20 people (5%) treated might find that their balance is not as good after treatment. We recommend that physiotherapy-rehabilitation might help.
There is a chance that your vestibular schwannoma might increase in size during the 4 years after treatment before reducing in size again. We will check and monitor this on follow-up scans.
If your hearing has been affected by the vestibular schwannoma you might have further hearing loss after treatment. However, this should be at a slower rate than if we left the tumour untreated.
Further supplies of your medicines
Prescriptions are now prescribed electronically. You will need to collect your medicines from our Guy's Pharmacy department so you have them ready to take from the morning of your first treatment.
Guys' Pharmacy location: ground floor, Tower Wing, Guy's Hospital, Great Maze Pond, London SE1 9RT. Phone: 020 7357 7583
GPs are now able to access your prescription from the London Care Record if you need further supplies.
Anyone with a cancer diagnosis is entitled to free prescriptions. You will need a medical exemption card. You can get an application form from your GP, the oncology outpatient department, or from Dimbleby Cancer Care on the ground floor.
At the end of your treatment
On the last day of treatment, you will be given a treatment completion form which summarises your treatment. We will also send a copy to your GP.
Follow-up
The stereotactic radiographer will call you 2 weeks after your treatment has finished to ask how you are.
After 6 weeks, an oncology consultant or a member of their team will call you to check how you are.
Radiotherapy takes time to work. It is important that your doctor assesses you, discusses your progress and any side effects with you.
If you have any concerns about your side effects, please contact one of the stereotactic radiographers. The number is in the Contact us box.
After your oncology consultant has called you, your care will continue under the hospital or department that you were referred from.
Improving our service
To help improve treatments and services, we regularly carry out audits. This can involve using patient notes. Any data collected will be confidential and all personal and identifiable details will be removed.
Please let your consultant know if you would prefer that your notes are not seen, and we will respect your wishes.
Clinical trials are undertaken within the department and you might be eligible to take part in. If necessary and appropriate, your doctor will discuss this with you.

