Overview
Chemotherapy infusion device
A chemotherapy infusion device administers chemotherapy medicine at a slow, continuous rate, over a set period of time. It is usually given if you are having chemotherapy treatment at home.
About your treatment
You will receive a type of chemotherapy medicine called 5-Fluorouracil (5FU).
You will need to have a central venous access device (CVAD) fitted, so that we can connect it to your infusion device. The CVAD delivers the medicine directly into your bloodstream, through a vein. We will give you information about this.
Your chemotherapy nurse will tell you how long you will need the infusion device for.
What the infusion device looks like
There are different types of infusion device. They deliver the medicine at different rates and volumes (amounts).
The device contains a small balloon that is filled up with your medicine. As the medicine is given, the balloon slowly shrinks (deflates).
The balloon is enclosed in a hard, plastic case for safety. It is about the size of a small water bottle, and has a tube so it can be carried in a pouch.
We will give you a device that is best suited to your treatment.
Using the device
Your nurse will attach the infusion device containing the chemotherapy to your CVAD. When attached, it will deliver the medicine slowly over several days.
You will receive a pouch and strap for carrying the device, which can be worn around your waist or over your shoulder.
The device may feel strange at first, but most patients adapt to it quickly. It should not interfere with your daily activities.
When the infusion is complete
A nurse will either visit your home or ask you to come to the clinic to disconnect the device.
The CVAD will be flushed with saline (saltwater) and secured.
CVAD maintenance, including flushing and dressing changes, is required every 7 days between treatments. The nurses will schedule this with you.
Monitoring progress
Your nurse will show you how to check the balloon size, and how you can check that the medicine is infusing correctly.
The balloon should gradually shrink over time. The markings on the outer case can help you to check this.
Check your device every 8 to 12 hours to see if the balloon is shrinking.
If the balloon does not shrink, you should read our information about what to do if there is a problem.
You might find these pictures helpful as a guide.
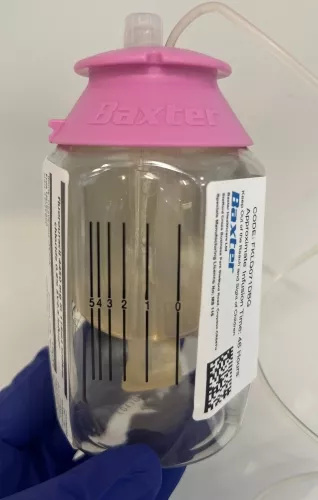
Full infusion device
The balloon is full, which means it contains the medicine.
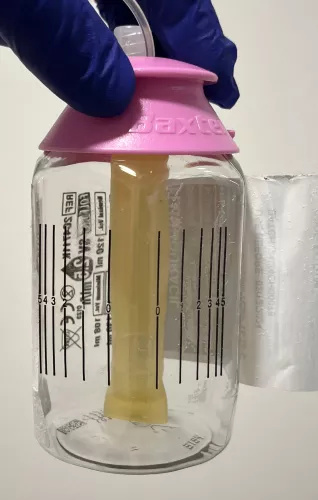
Empty infusion device
The balloon has deflated, which means the medicine has infused.
Care of your infusion device
Sleeping
- Do not place the device on the floor or above your head while you are sleeping. This can affect the flow. Place the device on a bedside table, or at a similar height.
- Make sure that the device does not become tangled in bedsheets, pillows or duvets, to avoid pulling on the CVAD.
Washing
- Protect the device during showers or baths by hanging it away from water.
- Use plastic coverings, like cling film, to keep the CVAD dry. Your GP can also supply this. We will give you more information about this when you have the CVAD fitted.
Exercising
You can exercise with the infusion device as long as it remains close to room temperature and is not exposed to water. Ask your doctor or nurse for more advice.
Travel
It is safe to travel on planes that have pressurised cabins when wearing your device. However, you should let your team know if you are planning on travelling abroad.
Pets
The device is safe to use around pets, but make sure it is protected from damage and chewing.
Safety
Your chemotherapy medicine will circulate through your body. It is then removed from your body through your bodily fluids, such as your pee (urine). This can be harmful to others.
It is important that you take extra care during this time.
- Make sure you flush the toilet with the lid down after you have used it.
- If bed sheets or covers become soiled with vomit, pee, or poo, they should be washed separately from other items. Wear gloves when you are removing any soiled items and avoid touching the contaminated areas.
- If you are sexually active, you or your partner should use condoms. This protects your partner from exposure to the chemotherapy medicine. This should continue for 48 hours after your chemotherapy has finished.
- Keep a bowl nearby in case you feel sick. If you are sick (vomit) and use a plastic bowl, it must be thoroughly washed with soapy water after use, and then disposed of when you have completed all your treatment. It should not be used for anything else.
Please contact the acute oncology unit if you are sick (vomit).
What to do if there is a problem
You should follow these instructions if you have any problems with your device, or if you need support.
- Put on disposable gloves.
- Check if the connection between the tubing and CVAD is loose. Gently make sure the connection is tight. Do not screw in too firmly or the connection may crack.
- Check for any visible cracks in the infusion device, tubing or CVAD.
- If you have located the leak, wrap the leak with gauze and tape.
- If your CVAD has a clamp, close the clamp on your line.
- Use warm, soapy water to wash any area on your skin, clothing, or furniture that the fluid has come into contact with.
- Contact your nurse to let them know what has happened.
Do not disconnect the device.
- If your CVAD has a clamp, check that the clamp is open.
- Check for kinks or folds in the line of the device and also on your CVAD.
- Contact your nurse to let them know what has happened.
Do not disconnect the device.
If you notice that the device has emptied before expected (hours or days earlier), contact your nurse.
If the district nurse has not arrived to disconnect your device, or to flush your line, please contact them directly. You can get their number from your GP.
If you cannot get through to them, call the Chemotherapy Village who can put you through to a nurse.
Side effects of chemotherapy
Some people have side effects, such as feeling sick, from having chemotherapy. You will have been given information about different side effects and what to do if you have them.
If you have any questions about side effects or have not been given information about this please speak to a member of staff caring for you.
Resource number: 4336/VER3
Last reviewed: November 2024
Next review due: November 2027
