Preparing and giving yourself bortezomib injections
Injecting the cancer medicine bortezomib yourself
A nurse in the chemotherapy day unit has shown you how to give yourself an injection under the skin. We have also prepared a short video on how to give yourself an injection. You may find it helpful to refer to this video while you get used to injecting bortezomib.
You need to follow this procedure to prepare and give yourself bortezomib injections.
Preparing the injection
- Remove the bortezomib syringe from the fridge and allow it to reach room temperature before injecting. This usually takes 15 to 30 minutes and reduces any discomfort from having the injection.
- Check the details on the label of your medicine. Make sure that the label has your name on it.
- Check that the contents of the syringe are clear and not discoloured. Make sure that the volume of the syringe matches what the label says.
- Check that the injection has not passed the expiry date on it.
- Collect all your equipment and put it on a clean surface.
- Wash your hands thoroughly with soap and water, and dry them.
- Remove and open the packets containing the syringe and the gauze swabs.
Giving yourself the injection
- Remove enough clothing to uncover the area that you are using for the injection. This could be your tummy (abdomen) or outer thigh. Take it in turns to inject into the left and right sides of your tummy or left and right thigh. You need to record the area (site) that you use for each injection in a table.
- Open an alcohol swab packet and take out the swab. This is a cotton pad soaked in alcohol to clean a patch of skin before an injection.
- If a carer is giving you the injection, they need to put on an apron and gloves.
- Use the alcohol swab to clean the skin where you plan to inject yourself. Let this area dry for 15 to 30 seconds.
- Take the plastic cover off the needle. Hold the syringe between your thumb and the finger next to it (index finger) of the hand that you write with. This is a similar position to holding a dart.
- With your free hand, gently pinch the skin of the area that you have chosen to inject. This raises the layer of tissue under your skin. If you can pinch 5cm (2 inches) of skin, insert the needle at a 90 degree angle to your tummy. If you can only pinch 2.5cm (1 inch) of skin, insert the needle at a 45 degree angle.
- When you have inserted the needle completely, slowly push the plunger down as far as it will go. Hold it there for at least 10 seconds to make sure that you have injected everything in the syringe.
After having the injection
- Remove the needle and put gentle pressure on the injection site with a gauze swab. This is a cotton pad for cleaning a patch of skin, including any leakage, after an injection. Do not massage the area.
- Cover the injection site with a plaster, if needed.
- Do not put the needle back into the needle cover.
- Put the used needle and syringe into the yellow sharps bin with a purple lid. When you have filled this to the line on the bin, close the lid. Return the bin to the hospital at your next visit or contact your local council to arrange collection.
- Wash your hands thoroughly with soap and water again, and dry them.
Areas where you can inject under the skin
You can inject bortezomib into:
- any area of your tummy (abdomen) that is about 2 to 5cm away from your belly button
- your outer left or right thigh
It is best to inject into a fatty area where you can pinch at least 2.5cm (1 inch) of skin.
Do not inject the medicine into skin that is broken, hardened, inflamed, swollen, bruised or damaged from a previous injection. If you are not sure, choose a different site or ask your nurse for advice.
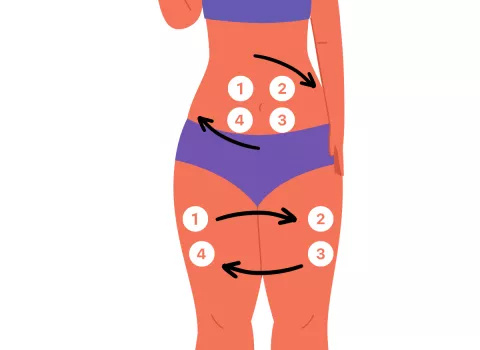
Changing (rotating) your injection site
If you inject into the same area too many times, fatty lumps can appear on the surface of your skin. This can make injections more difficult and painful.
To avoid this problem, choose a different place (site) and area of skin for each injection. You can inject bortezomib into your tummy (abdomen) or outer thighs.
It is important to:
- take it in turns to inject into the left and right sides of your tummy or outer left and right thigh
- choose a different area of skin each time
- keep each new injection spot at least 2.5cm (1 inch) away from the previous injection site
The following diagram shows how to rotate your injection site between different areas of the body.
You can download and print the following PDF document or ask staff in the chemotherapy day unit for a paper copy. This document has a table for you to record the site that you use for each injection. Please bring the completed document to your next hospital appointment.
If you miss a bortezomib injection
Contact us for urgent advice if:
you miss a prescribed amount (dose) of bortezomib for any reason. Your clinical nurse specialist or the chemotherapy day unit can explain what to do.
If you want to stop giving yourself injections
If you want to stop giving yourself injections or there are reasons why this becomes unsafe, contact your clinical nurse specialist or the chemotherapy day unit.
You can start having treatment again in the chemotherapy day unit. A nurse here can give you the injections instead if this suits you better.
You need to return any unused bortezomib syringes to the chemotherapy day unit. We can then dispose of them safely.

